
What Are Bedsores and How Can You Prevent Them?
Bedsores are a serious but preventable complication. When someone becomes bedridden due to chronic illness, aging, recovery from surgery, or a disability, their risk for developing bedsores increases significantly. For caregivers, family members, and patients, understanding bedsore prevention is an essential aspect of long-term care.
What causes bedsores?
Bedsores are caused by prolonged pressure from one position, as this can reduce blood flow and oxygen to the tissues, making the skin vulnerable to breakdown. Additionally, consistent friction between the skin and sheets or clothing can contribute to skin breakdown.
Bedsores are more common in bony parts of the body, like the back of the head, shoulder, elbows, lower back, buttocks, and heels of your foot. For people who spend most of their time lying in bed, these areas bear the most pressure and require close attention.
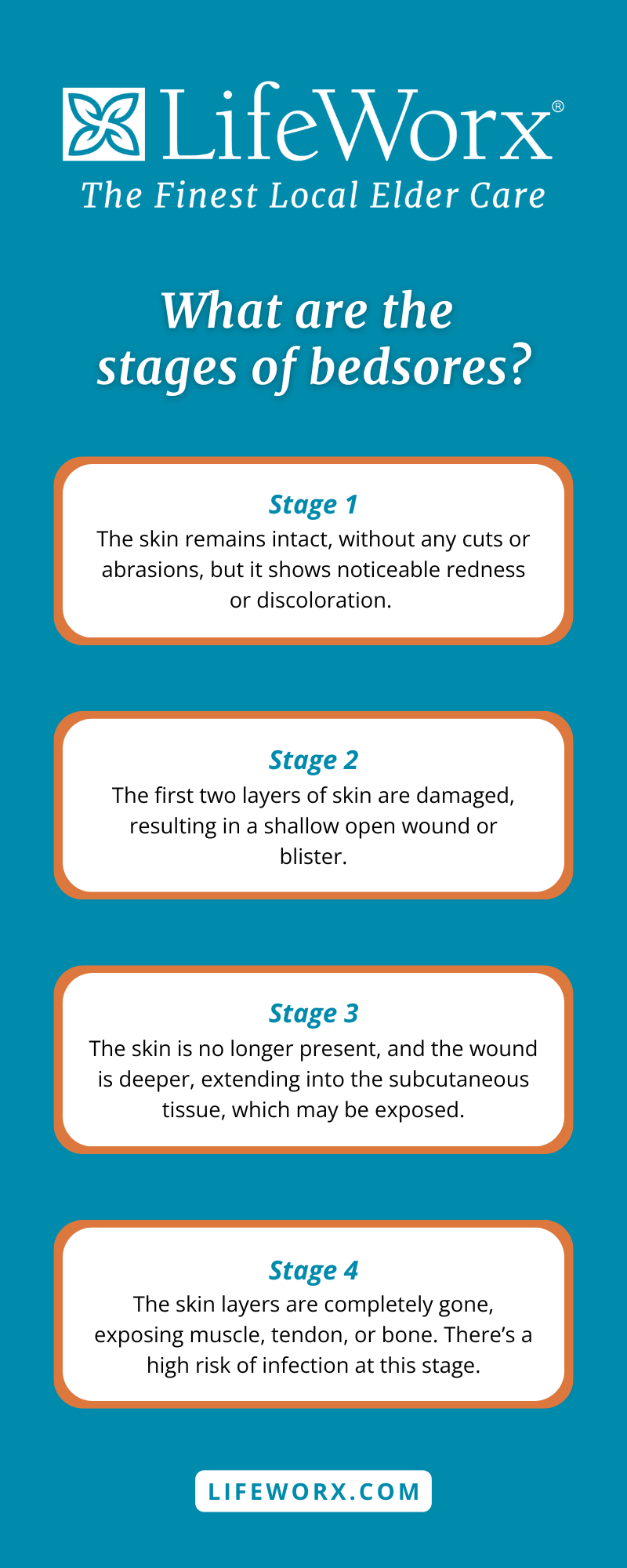
Stages of bedsores
Bedsores develop in four stages, each more severe than the last. They begin with mild redness in the affected area, which, if left untreated, can lead to skin loss with an open wound, exposing muscle, tendon, or bones.
Stage 1: The skin remains intact, without any cuts or abrasions, but it shows noticeable redness or discoloration.
Stage 2: The first two layers of skin are damaged, resulting in a shallow open wound or blister.
Stage 3: The skin is no longer present, and the wound is deeper, extending into the subcutaneous tissue, which may be exposed.
Stage 4: The skin layers are completely gone, exposing muscle, tendon, or bone. There’s a high risk of infection at this stage.
A healthcare professional, such as a medical doctor, registered nurse, or wound specialist, can assess the severity of the bedsores and recommend an appropriate course of treatment.
How to identify a bedsore
Inspections of the skin are one of the most important habits caregivers can develop. Signs of a bedsore include:
- Redness or discoloration that does not turn white when pressed
- Increased warmth or coolness around the discolored area
- Pain or discomfort in the affected region
- Blisters forming where there has been prolonged pressure or friction
Bedsore prevention strategies
Preventing bedsores in bedridden patients involves reducing the pressure on the skin, especially in bony areas. Here are some effective strategies:
Repositioning: Changing positions at least every two hours to increase blood flow and bring oxygen back to the tissues.
Exercise: Passive exercises can stretch and strengthen joints to increase mobility.
Pressure relief: Use pillows or foam to cushion the bony areas and provide relief.
Hydration and moisture: Drink lots of water and keep the skin moisturized to prevent dryness and skin breakdown. This can decrease your risk of bedsores and wounds.
Preventing bedsores is an important part of caring for someone who is bedridden. With careful attention to movement, skin care, and comfort, most bedsores can be avoided. For those who need additional support, LifeWorx can provide experienced caregivers to maintain these routines. Caregivers can assist with personal and companion care to help prevent bedsores or care for any existing ones. Caregivers can change your position, adjust pillows and cushions, remind you to stay hydrated, and give bed baths followed by skin moisturizing.
Having the right care in place can make a big difference in prevention and quality of life. If you’re interested in learning more about our in-home care services, get in touch with our team today.


















