
Incontinence Care in The Elderly
Incontinence is a common issue in older adults caused by a variety of factors, including age-related changes, medical conditions, and side effects. Incontinence refers to the involuntary loss of bladder and bowel control, which can significantly impact daily activities and cause emotional distress. However, by recognizing the signs and understanding the types of incontinence, seniors, their caregivers, along with healthcare providers, can make it easier to manage.
Symptoms of incontinence
The symptoms of incontinence can vary from person to person. For some, it may be a small leak when they laugh or sneeze. Others may feel a sudden urge to go and not enough time to make it to the bathroom. These symptoms may come and go, or they may become more frequent over time.
Incontinence can manifest in various ways, depending on its cause and type. Common signs that may indicate a problem with bladder control include:
- Bedwetting in older adults
- Leaking urine during physical activity
- Dribbling urine, even after using the bathroom
- Frequent urination, including waking up several times at night
- Sudden urge to urinate that isn’t easy to control
If any of this sounds familiar, it’s worth looking into. These symptoms are not part of regular aging and recognizing the early signs of incontinence can help prevent complications and improve outcomes.
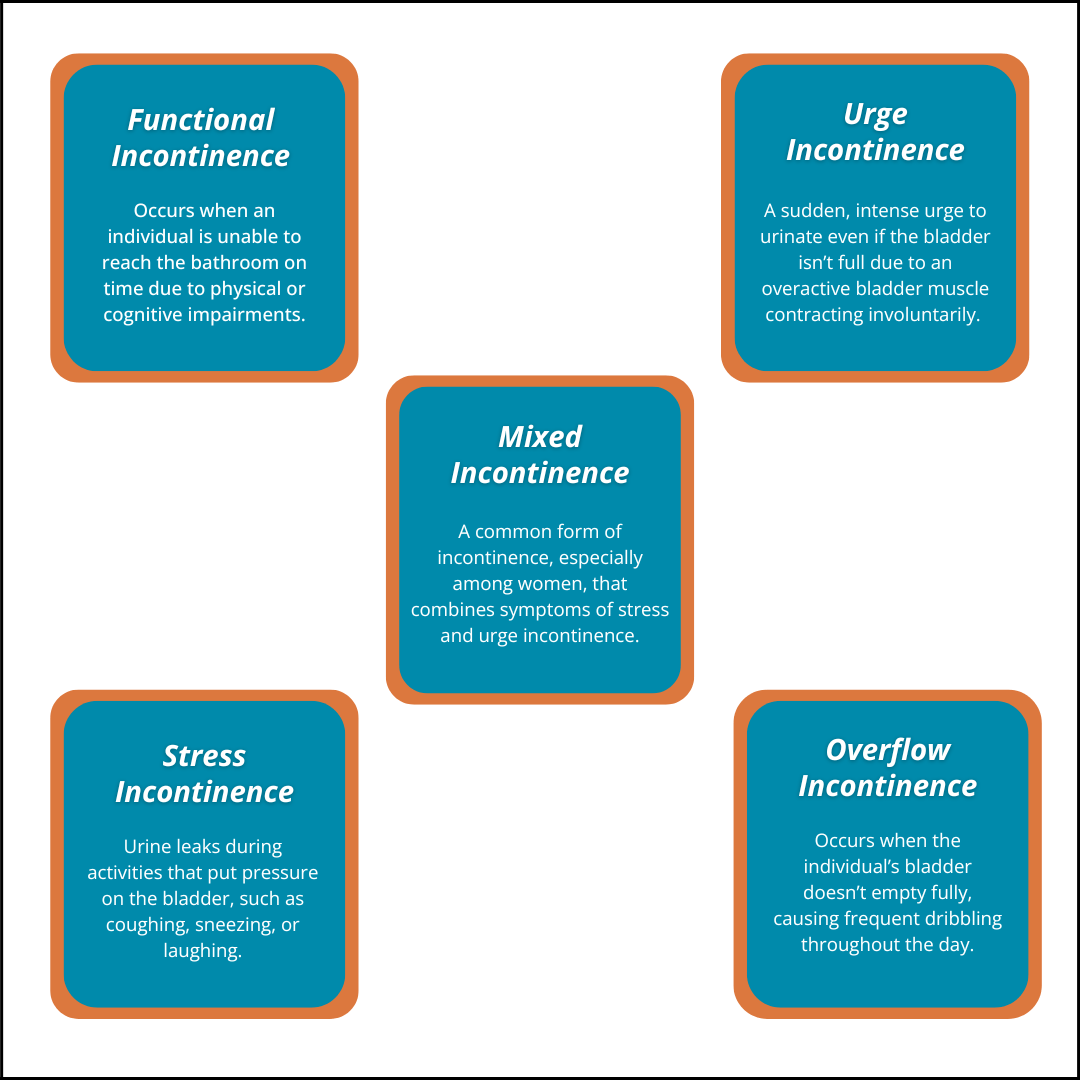
Types of incontinence
Incontinence affects people in different ways. Understanding the type of condition your loved one is dealing with can make it easier to find the right support and treatment.
Functional incontinence happens when someone can’t get to the bathroom in time, even though their bladder is working normally. It’s often related to physical limitations, such as difficulty walking due to arthritis, a stroke, or general weakness. Cognitive conditions, such as dementia, can also make it harder to recognize the need to use the bathroom or remember where it is. Sometimes the environment itself plays a role, for instance, stairs, long distances to the bathroom, or low toilet seats.
Planning ahead is a common strategy for addressing functional incontinence. Bathroom visits might be scheduled at regular times to anticipate needs. Keeping a commode or urinal nearby can help, especially at night. Simple modifications in the home, like adding a raised toilet seat or ramp, can make life more manageable.
Stress incontinence occurs when pressure is placed on the bladder during activities such as coughing, sneezing, laughing, or lifting something heavy. It’s usually caused by weakened pelvic floor muscles. This can happen after childbirth, as people age, or when there is added pressure on the bladder from body weight or frequent coughing.
Treatment often begins with exercises to strengthen the pelvic floor, such as Kegels. Adjusting fluid intake and reaching a healthy weight can also reduce pressure on the bladder. Some people may benefit from medications that support muscle control.
Urge incontinence involves a sudden, strong need to urinate, typically followed by leakage. It’s usually linked to an overactive bladder, where bladder muscles contract even when they shouldn’t. This can happen due to nerve damage from conditions like stroke or multiple sclerosis. Bladder irritation or an enlarged prostate can also be factors.
To manage this type of incontinence, it’s helpful to limit bladder irritants such as caffeine and alcohol. Medications that relax the bladder muscles may be prescribed, and in some cases, Botox injections can help reduce muscle contractions. Protective pads can be particularly helpful, especially at night.
Overflow incontinence occurs when the bladder doesn’t empty completely, resulting in frequent leaks or dribbling. It can be caused by a blockage that slows urine flow, such as an enlarged prostate or pelvic organ prolapse. Weak bladder muscles, sometimes related to diabetes or spinal injuries, can also be the cause.
Treatment focuses on helping the bladder empty completely. Medications may be used to improve urine flow, and pelvic floor exercises can also offer support. Timed bathroom visits can help avoid overfilling. In some situations, a catheter can also be used to help drain the bladder.
Mixed incontinence means more than one type is happening at the same time. The most common combination is stress and urge incontinence. Because there’s more than one cause, treatment usually involves a combination of strategies.
Once the type of incontinence is determined, appropriate medications, lifestyle changes, and environmental modifications can be implemented to manage and alleviate symptoms. For older adults managing incontinence, consistent support in the home can make a significant impact.
LifeWorx has a team of dedicated Registered Nurses who can assess body function and the home environment, offering recommendations for caregivers to improve the quality of life for seniors. Contact our team if you would like to learn more.


















